


Radio-iodine Therapy: For over 50 years now, radioiodine has remained one of the most useful radio-isotope for diagnosis and therapy in Nuclear Medicine. The wide application of radioiodine in the study of the thyroid gland and in the management of its disorders has been most rewarding. This treatment is safe, well tolerated and has successfully treated many cases of hyperthyroidism and thyroid cancer even after the tumor has spread.
Every Saturday to Thusday at 8.00am -2.30pm
Except Friday and all government holiday
Every Saturday to Thusday at 7.30 AM
Except Friday and all government holiday
| Invastigations | Rate | Preparation |
|---|---|---|
| Post-operative thyroid ablation with I-131 for differentiated thyroid Cancer (100 mCi) | 10000 | Get Appointment |
| Post-operative thyroid ablation with I-131 for differentiated thyroid Cancer 200mCi | 20000 | Get Appointment |
| Post-operative thyroid ablation with I-131 for differentiated thyroid Cancer 30 mCi | 4000 | Get Appointment |
| Initial assessment for RA 1-131 Therapy | 350 | Get Appointment |
| Book Charge | 100 | Get Appointment |
| Post-operative thyroid ablation with I-131 for differentiated thyroid Cancer 50 mCi | 6000 | Get Appointment |
| Post-operative thyroid ablation with I-131 for differentiated thyroid Cancer 150 mCi | 15000 | Get Appointment |
| Radioiodine treatment for grave's disease, Toxic thyroid nodule and Multinodular toxic goiter | 2000 | Get Appointment |
| Free T4 (FT4)/ Thyroxine (T4) | 600 | Get Appointment |
| T4+ TSH (Only for therapy follow up patients) | 1000 | Get Appointment |
| Tg | 700 | Get Appointment |
| Post-operative thyroid ablation with I-131 for differentiated thyroid cancer (75-mCi) | 8000 | Get Appointment |
 ⇛ Nuclear Medicine uses small amounts of radioactive material to diagnose, evaluate or treat a variety of diseases. These include many types of cancers, heart disease, gastrointestinal, endocrine or neurological disorders and other abnormalities. Because nuclear medicine exams can pinpoint molecular activity, they have the potential to identify disease in its earliest stages. They can also show whether a patient is responding to treatment.
⇛ Nuclear Medicine uses small amounts of radioactive material to diagnose, evaluate or treat a variety of diseases. These include many types of cancers, heart disease, gastrointestinal, endocrine or neurological disorders and other abnormalities. Because nuclear medicine exams can pinpoint molecular activity, they have the potential to identify disease in its earliest stages. They can also show whether a patient is responding to treatment.
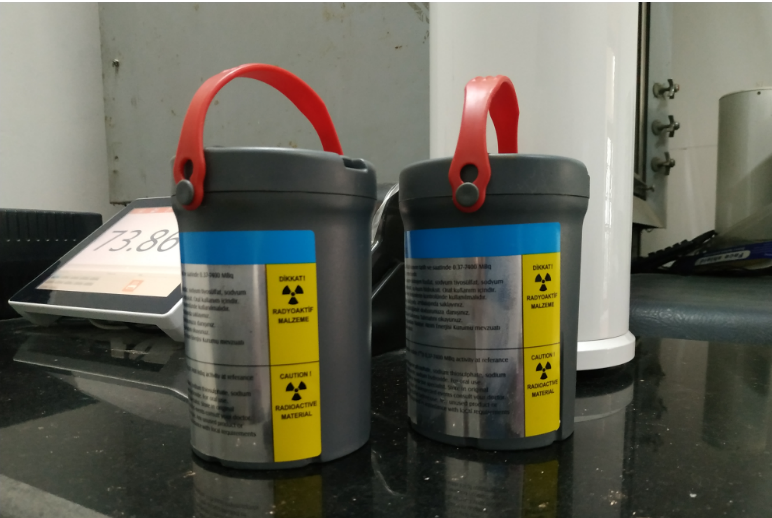
⇛ Radioactive Iodine 1-131 therapy (also called Radioiodine 1-131: an isotope of iodine that emits radiation) is a treatment for an overactive thyroid, a condition called Hyperthyroidism. Hyperthyroidism can be caused by Graves' disease, in which the entire thyroid gland is overactive, or by nodules within the gland which are locally overactive in producing too much thyroid hormone.
⇛ Radioiodine therapy is a nuclear medicine treatment for an overactive thyroid, a condition called hyperthyroidism, and also may be used to treat thyroid cancer. When a small dose of radioactive iodine l-131 (an isotope of iodine that emits radiation) is swallowed, it is absorbed into the blood stream and concentrated by the thyroid gland, where it begins destroying the gland's cells.
Radio-iodine Therapy:-
Radioactive Iodine (RAI) can be used for the treatment of overactive thyroid (Hyperthyroidism) and certain types of thyroid cancer (Differentiated carcinoma of thyroid - papillary and follicular). The term “radioactive” may sound frightening, but it is a safe, generally well-tolerated, and reliable treatment that targets thyroid cells so there is little exposure to the rest of the body’s cells.
What is hyperthyroidism ?
The thyroid gland , located at the front of your neck, makes hormones that control your metabolism—the way your body uses energy. Hyperthyroidism, also called overactive thyroid, occurs when your thyroid gland makes too much thyroid hormone. Too much thyroid hormone speeds up many of the body’s functions. If untreated, an overactive thyroid can lead to other health concerns, such as heart problems.The most common cause of hyperthyroidism is Graves’ disease, in which the immune system stimulates the thyroid gland. Less often, hyperthyroidism occurs when the thyroid has one or more nodules (lumps) that make too much thyroid hormone.
What is the treatment of hyperthyroidism ?
The goal of treatment is to lower the amount of thyroid hormones in the body. Treatment options include:
How does Radioactive iodine treatment work ?
The thyroid gland uses iodine to make thyroid hormone. It absorbs the iodine from the foods we eat. Similarly, the thyroid gland absorbs the RAI when it swallowed.Then, the radiation attached to the iodine damages the thyroid cells. Over time, the thyroid gland produces less thyroid hormone. Because no other organ in the body use iodine, the RAI does not affect any other part of the body. RAI, also called iodine 131 (I-131), is given as a single-dose capsule or liquid. Most often, for the treatment of hyperthyroidism you will not need to stay in the hospital. It can take 6 weeks to 6 months to see the full effects of RAI treatment. During this time, your thyroid blood levels will be monitored regularly. You may also need to take anti-thyroid drugs.
Who should not receive Radio-iodine Therapy?
For safety reasons, these people should not get RAI treatment:
Radio-iodine (RAI) is administered in Differentiated carcinoma of thyroid after total thyroidectomy for several reasons:
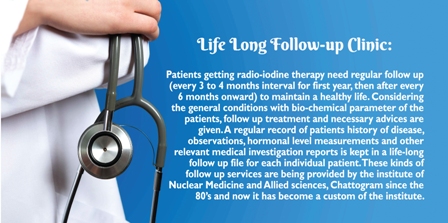
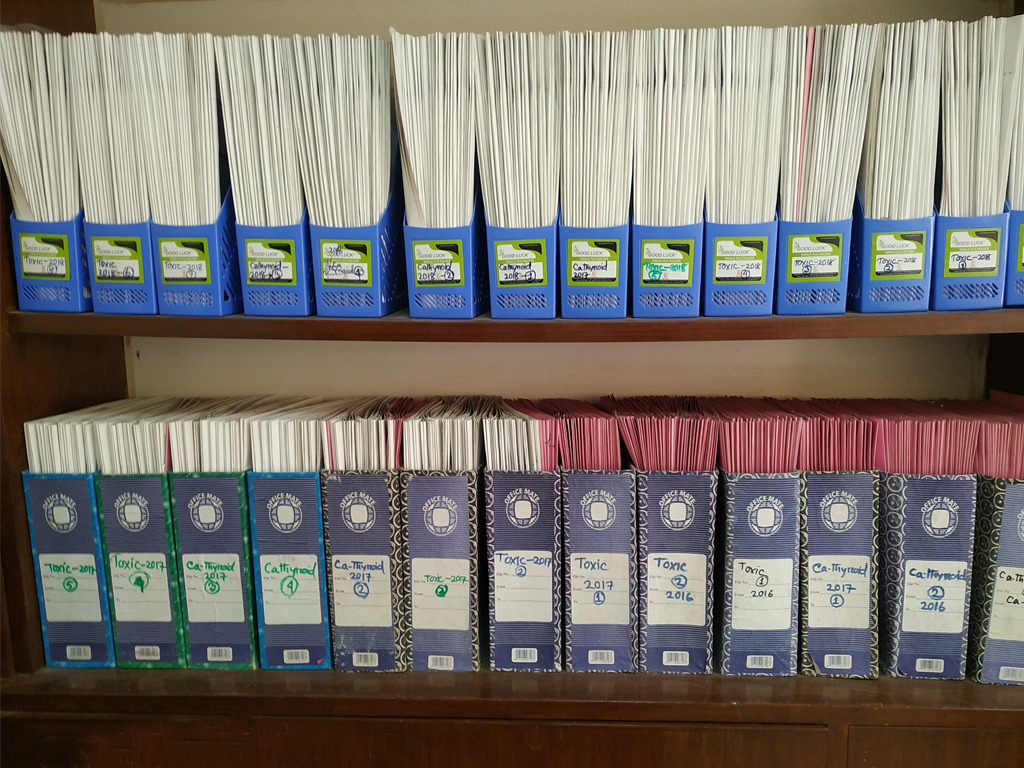
We have introduced patient ID card for our ‘Life-long Follow-up Clinic’ patients for -
1. Rapid patient identification
2. Prompt administrative procedure (Registration, Payment etc.)
3. Electronic Medical Record Management
4. Raised quality of care
Our ‘Life-long Follow-up Clinic’ includes patients of -
a) Hyperthyroidism
b) Hypothyroidism
c) Post-radioiodine therapy for hyperthyroidism
d) Post-radioiodine therapy for Differentiated Ca-Thyroid
Follow-up care:
Care should be given to a patient over time after finishing treatment for a disease. Follow-up care involves regular medical checkups, which may include a physical exam, blood, bio-chemical, hormone and imaging tests. Follow-up care checks for health problems that may occur months or years after treatment ends, including the development of other types of disease. In cancer patients, one purpose of follow-up care is checking to see if the cancer has come back or has spread to other parts of the body.
Contact us now to schedule an appointment.